Rafal Nowak, MD, PhD
Department of Ophthalmology, Military Institute of Medicine, Warsaw,
Poland
Correspondence to:
drrafal007@gmail.com
Aim
To present successful outcome of endoscopic endonasal dacryocystorhinostomy (EnDCR) in posttraumatic lacrimal drainage obstruction caused by the Le Fort fractures.
Introduction
Dacryocystorhinostomy (DCR) refers to the creation of a functional pathway for tears to drain into the nasal cavity by means of making an osteotomy and opening the lacrimal sac directly into the nasal cavity1. This kind of surgery is indicated in cases of nasolacrimal duct obstruction (NLDO), which can further cause chronic dacryocystitis with acute episodes2 (Fig.1). The procedure can be performed via an external or endoscopic endonasal approach. Some surgeons conduct laser-assisted transcanalicular DCR, although it does not provide good results3. DCR in primary acquired NLDO is a standard treatment, however, in posttraumatic cases it may turn out challenging.

Figure 1. Acute dacryocystitis.
Secondary posttraumatic NLDO usually results from a high-impact blunt facial trauma causing naso-orbito-ethmoidal (NOE) fractures, often being a part of the Le Fort fractures4, 5 (Fig.2-3). Since the upper lacrimal pathway is protected by the medial canthal ligament, lacrimal obstruction usually occurs in the bony nasolacrimal canal. Consequently, the anatomy of the lacrimal fossa and nasolacrimal duct (NLD) is altered with a lot of scarring, and the surgery carries an increased risk of failure. Some studies prefer external DCR or dacryocystectomy (DCT; removal of the lacrimal sac) in complex posttraumatic cases of NLDO6. They discourage endoscopic endonasal or laser DCR due to the loss of bony anatomical landmarks after trauma7.
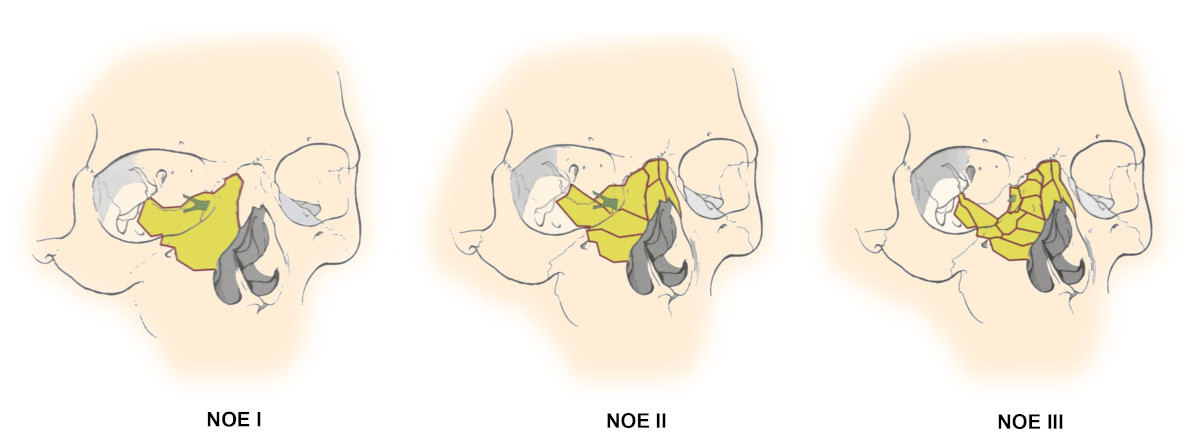
Figure 2. Types of NOE fractures8.
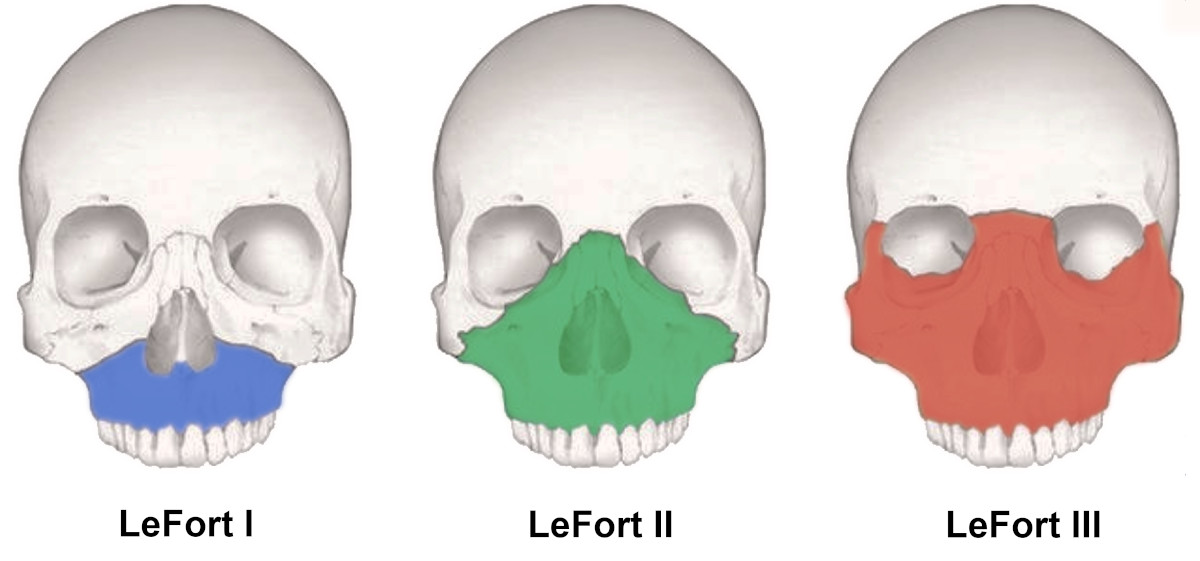
Figure 3. Types of Le Fort fractures9.
Materials and methods
This study refers to 3 cases of secondary posttraumatic nasolacrimal duct obstruction following Le Fort fractures. The surgeries of EnDCR were performed at the Department of Ophthalmology of the Military Institute of Medicine in Warsaw within the period of 1.5 years: November 2020 - May 2022. The follow-up time was 1-2.5 years.
Apart from standard dacryological examination, extended imaging of computed tomography-dacryocystography (CT-DCG) was conducted. The images were analyzed in Osirix MD radiological software (Pixmeo SARL, Switzerland). For further evaluation and surgical planning Medical Imaging XR (Medicalholodeck AG, Switzerland) was used. Then, 3D reconstructions were made using the following processes:
STL* 3D model extraction from OsiriX MD STL* model cleaning, repairing, simplification and modification with MeshLab (Visual Computing Lab, ISTI-CNR, Italy) final processing in Blender (Blender Foundation, Netherlands) and obtaining color 3D models *STL - 3D file format
After careful analysis of all collected data, the surgeries were performed (Fig. 4-11).
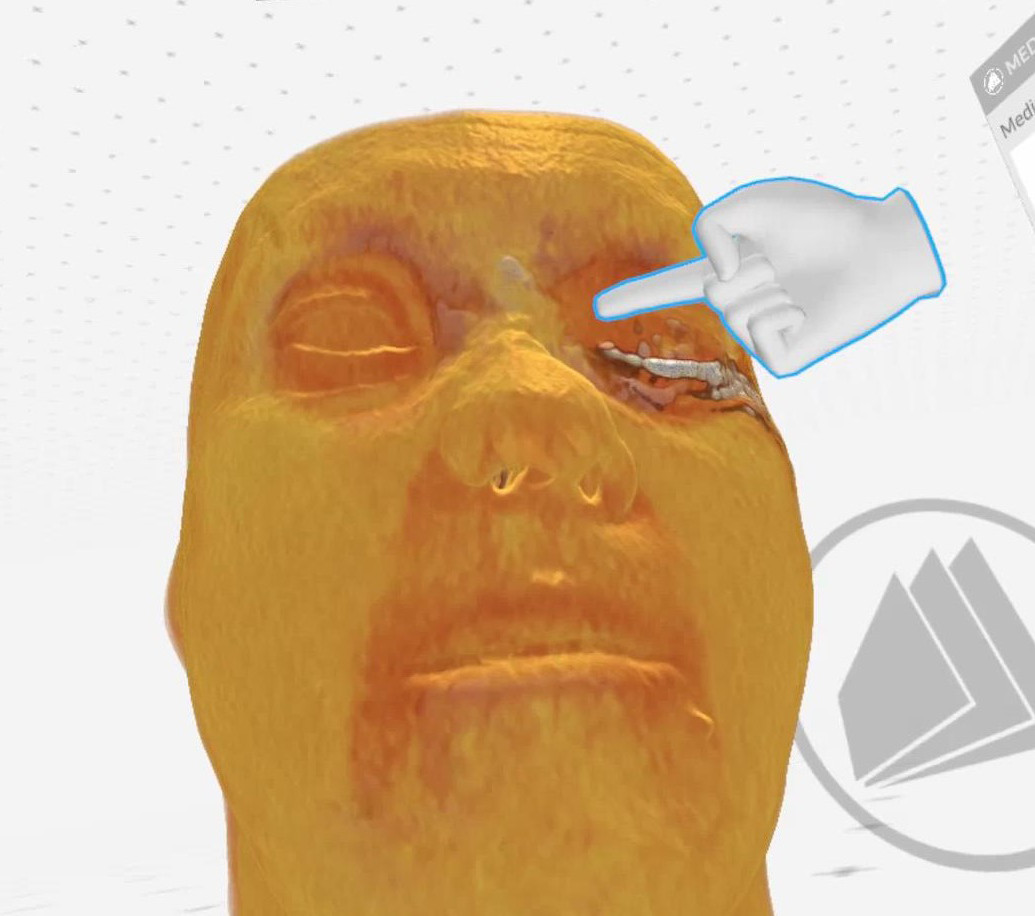
Figure 4. Case 1 (left side): Saddle nose (Medical Imaging XR reconstruction).
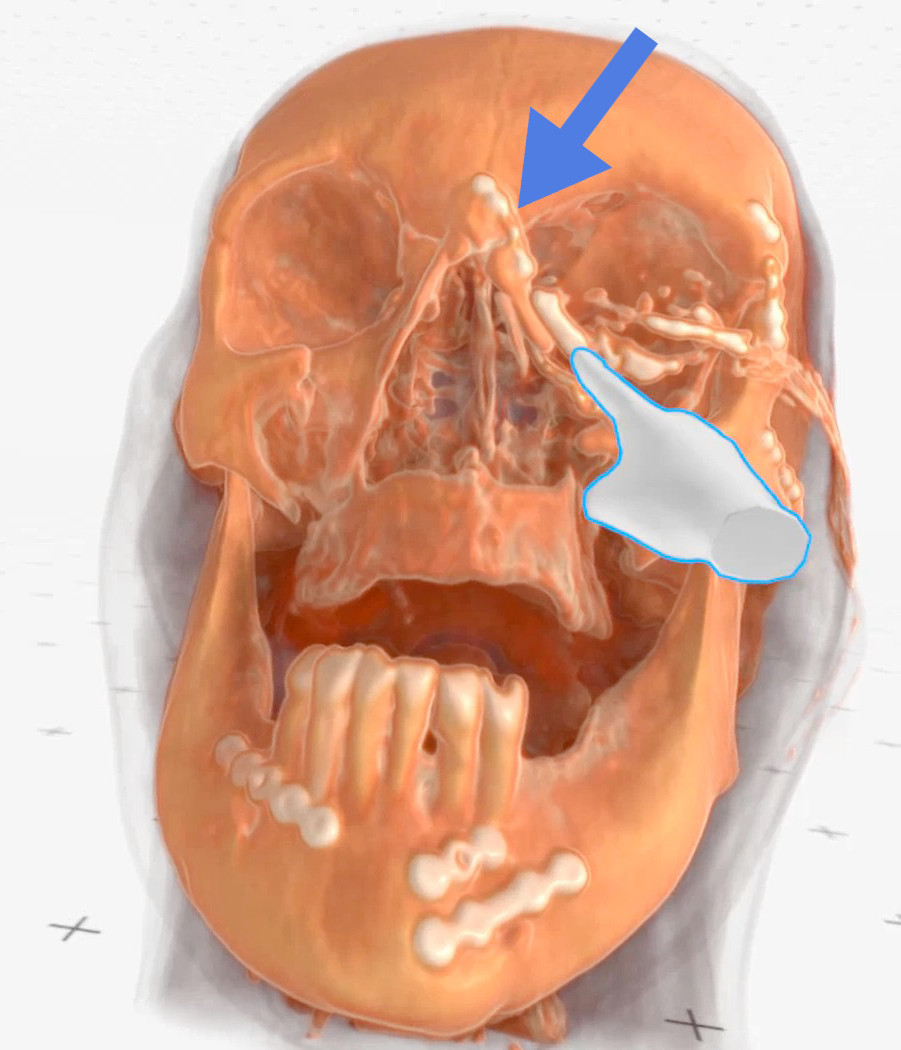
Figure 5. Case 1 (left side): Finger points at the lacrimal sac, blue arrow - indicates a metal plate neighboring the lacrimal sac (Medical Imaging XR reconstruction).
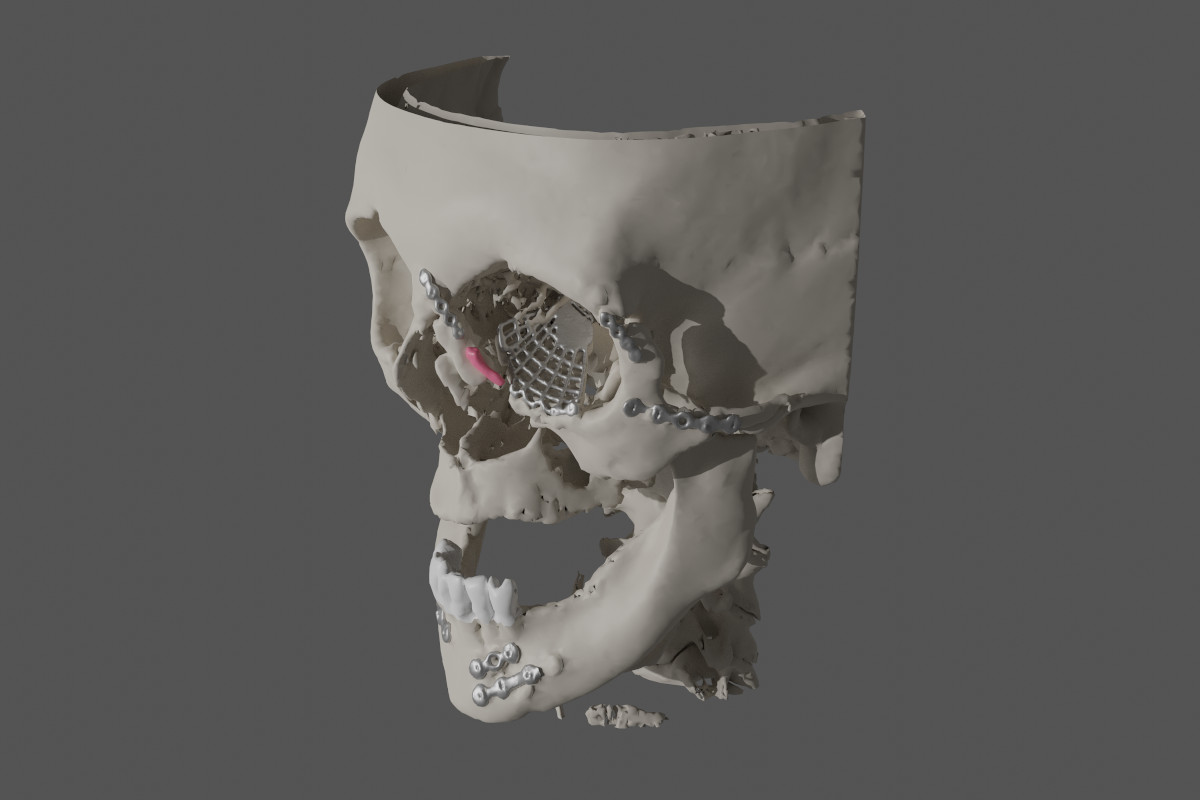
Figure 6. Case 1 (left side): Numerous metal plates and an orbital mesh; lacrimal sac marked in pink (reconstruction made with OsiriX MD/MeshLab/Blender).
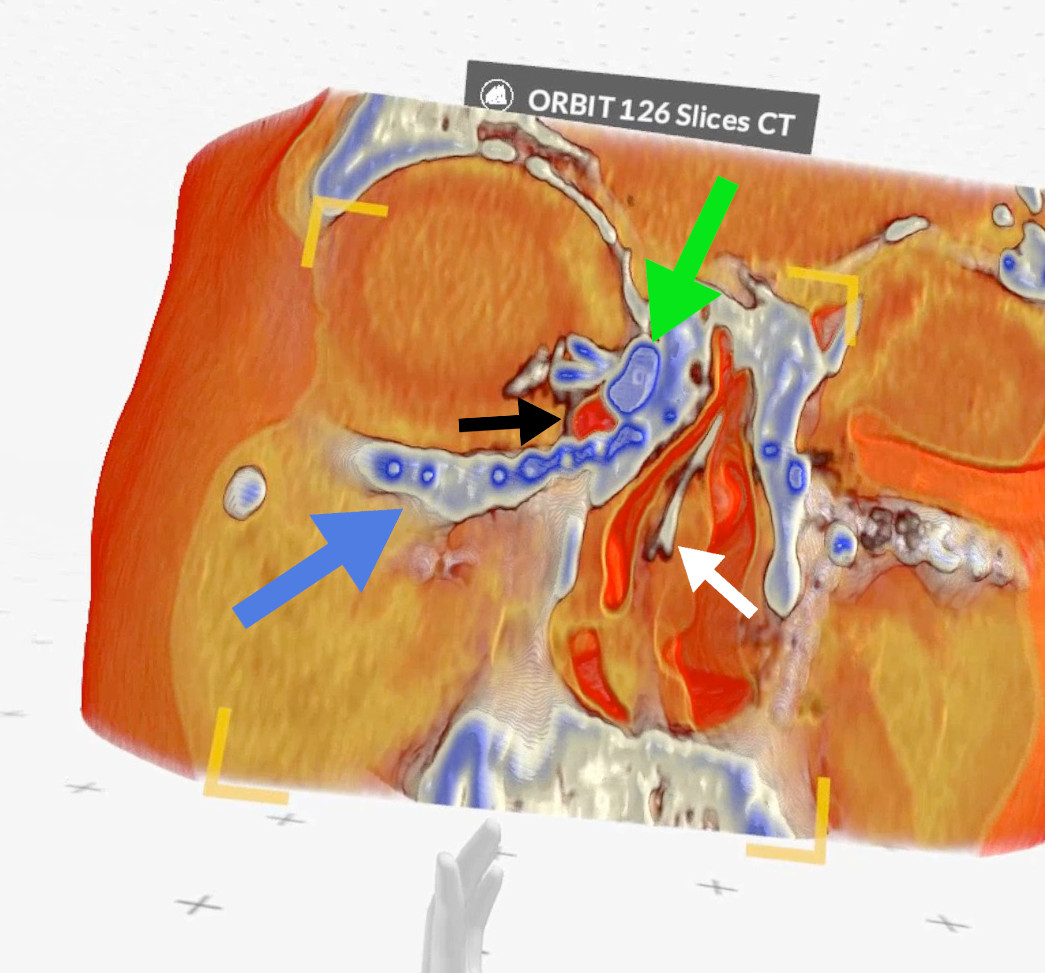
Figure 7. Case 2 (right side): green arrow - lacrimal sac, black arrow - air bubble inside the lacrimal sac, blue arrow - metal plate, white arrow - septal deviation (Medical Imaging XR reconstruction).
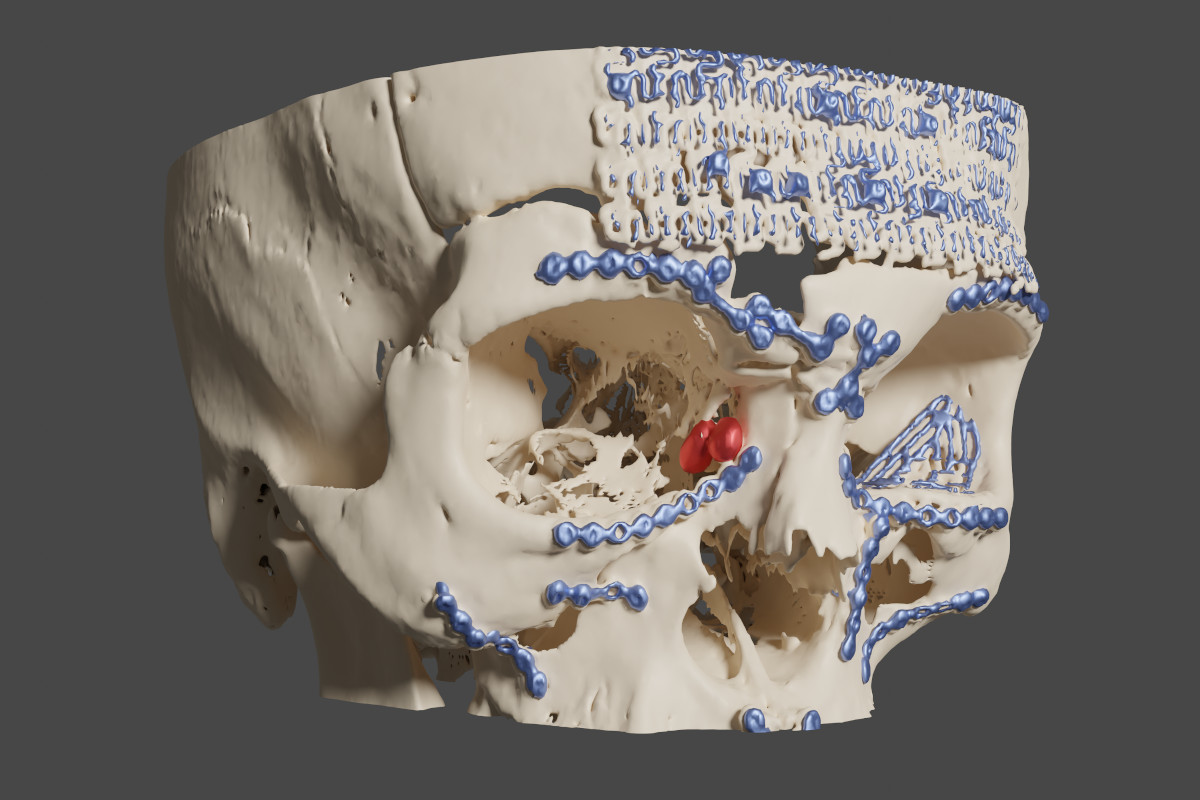
Figure 8. Case 2 (right side): blue - metal plates and meshes, red - lacrimal sac (reconstruction made with OsiriX MD/MeshLab/Blender).
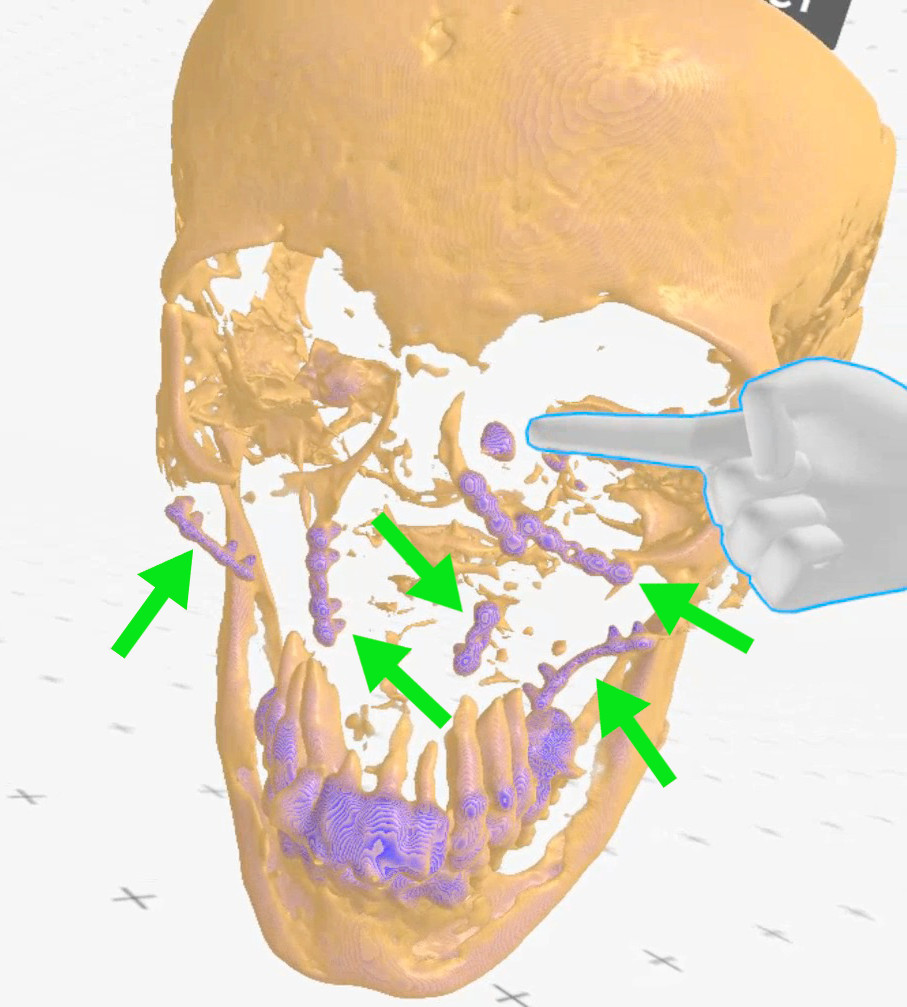
Figure 9. Case 3 (left side): finger points at the lacrimal sac, green arrows - metal plates (Medical Imaging XR reconstruction).
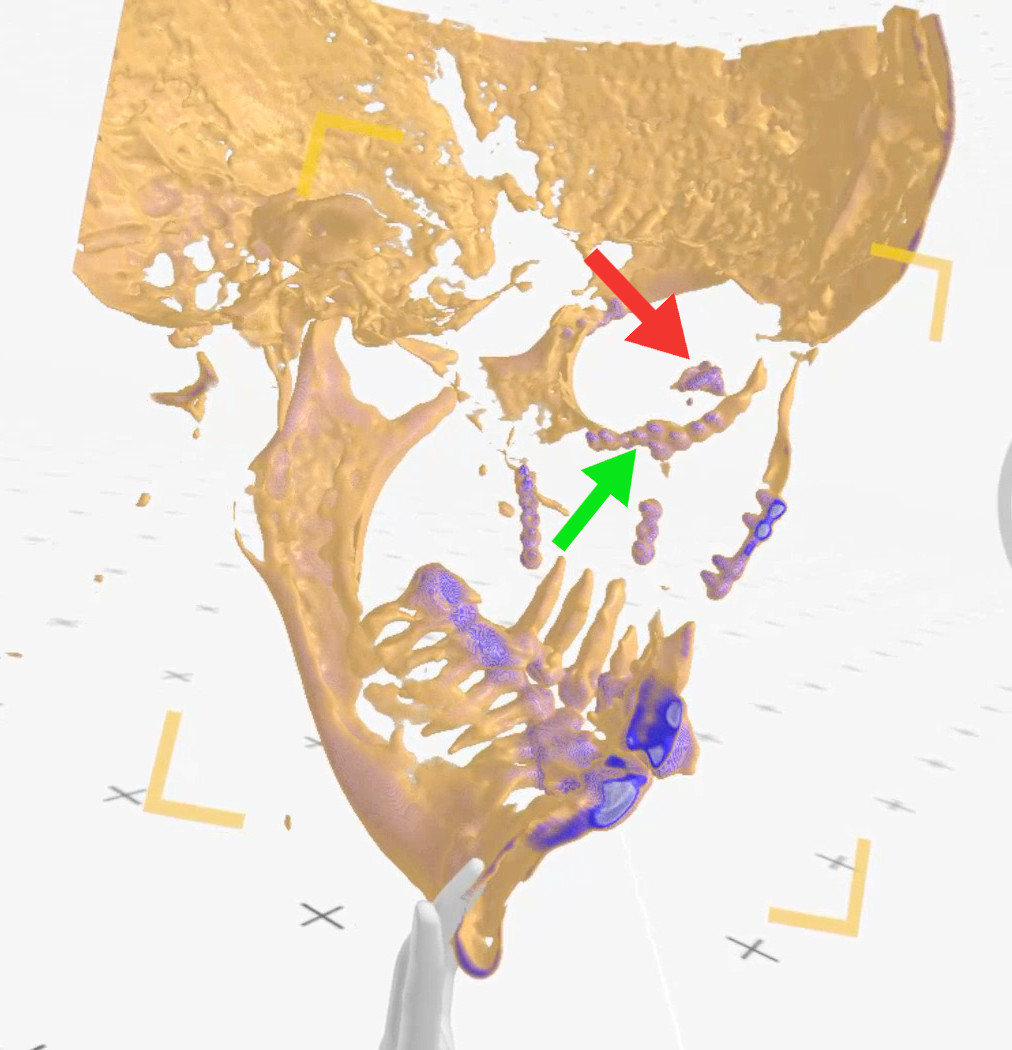
Figure 10. Case 3 (left side): view from inside the skull (from right to left), red arrow points at the lacrimal sac, green arrow - indicates metal plates neighboring the lacrimal sac (Medical Imaging XR reconstruction).
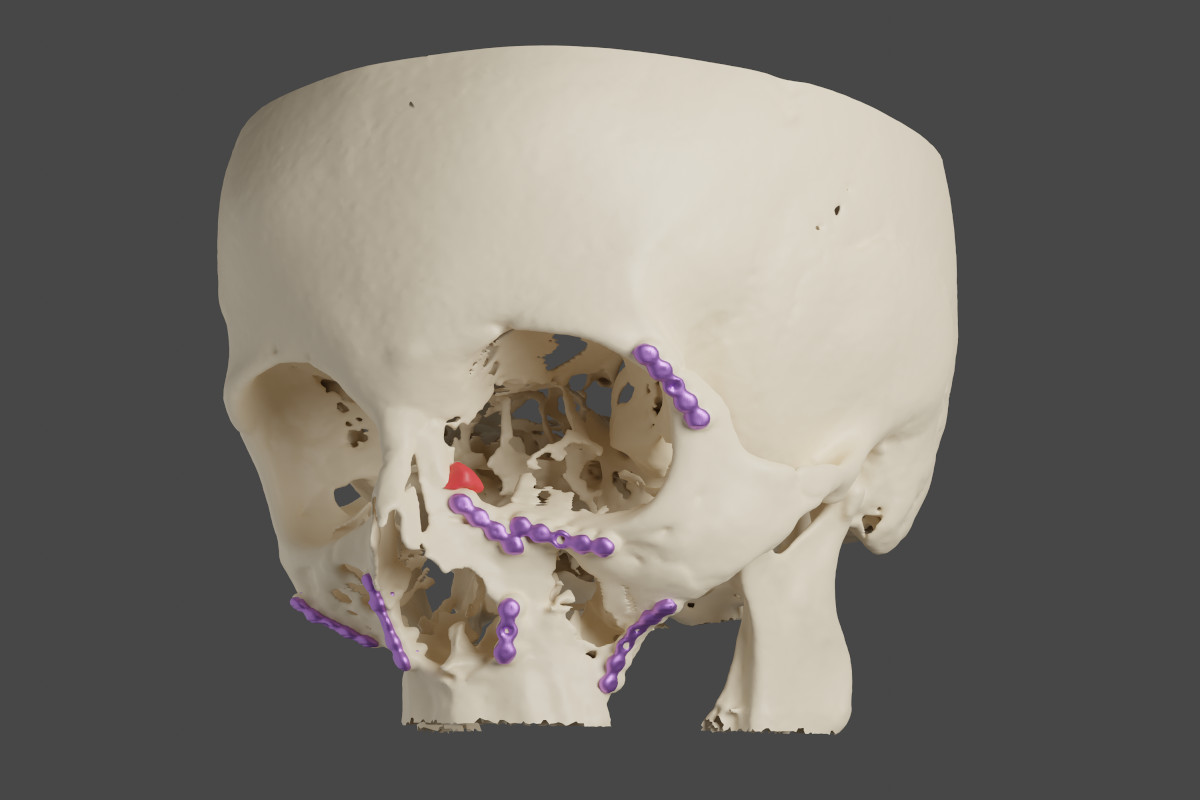
Figure 11. Case 3 (left side): red - the lacrimal sac, violet - metal plates (reconstruction made with OsiriX MD/MeshLab/Blender).
Surgical procedure of EnDCR The surgical procedure was conducted as described elsewhere10, 11, however, there were some derogations in each operated case. In all of them, light navigation was used to find the location of the lacrimal sac. Cases 1 and 2 had posttraumatic saddle noses and septal deviations.
CASE 1
The procedure was performed on the left side. The lacrimal sac was found under a thick layer of scar tissue, around 15mm anteriorly to the base of the middle turbinate. Thanks to the previous 3D visualization, it was known that a rim of a metal orbital mesh was located close to the middle turbinate (Fig. 12). It came to the surface during dissection but was then covered with a mucosal flap and tissue glue.
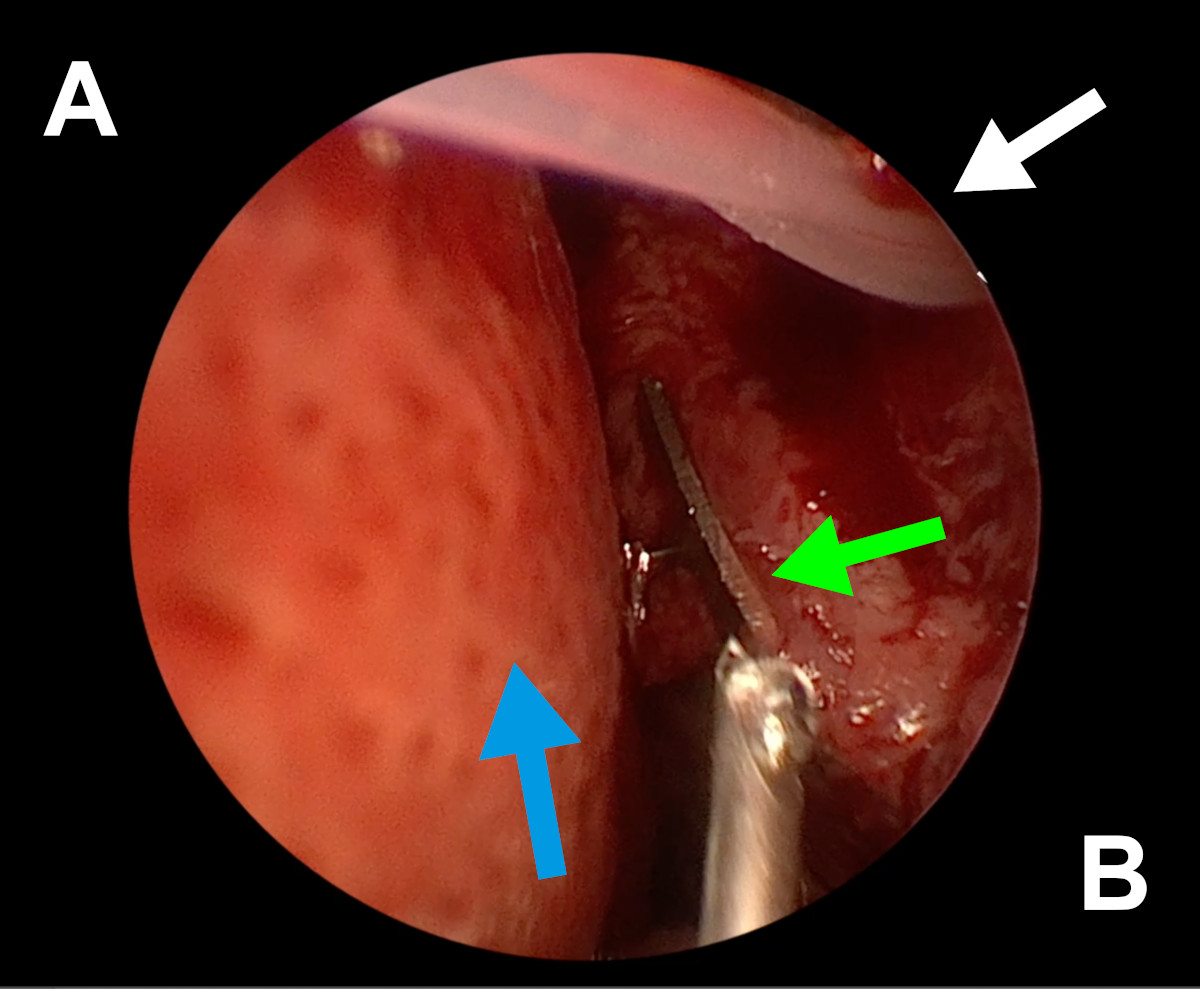
Figure 12. Endoscopic view of the left nasal cavity: white arrow – a silicone stent coming out from ostium, green arrow – orbital mesh, blue arrow – septal deviation (A- septum, B- lateral wall of the nasal cavity).
CASE 2
The procedure was performed on the right side. While fashioning the osteotomy, a tip of a metal bone screw was uncovered on its anterior edge. It had been expected, so burring was conducted around it in such a way that the neighboring nasal mucosa was able to cover it (Fig. 13-15).
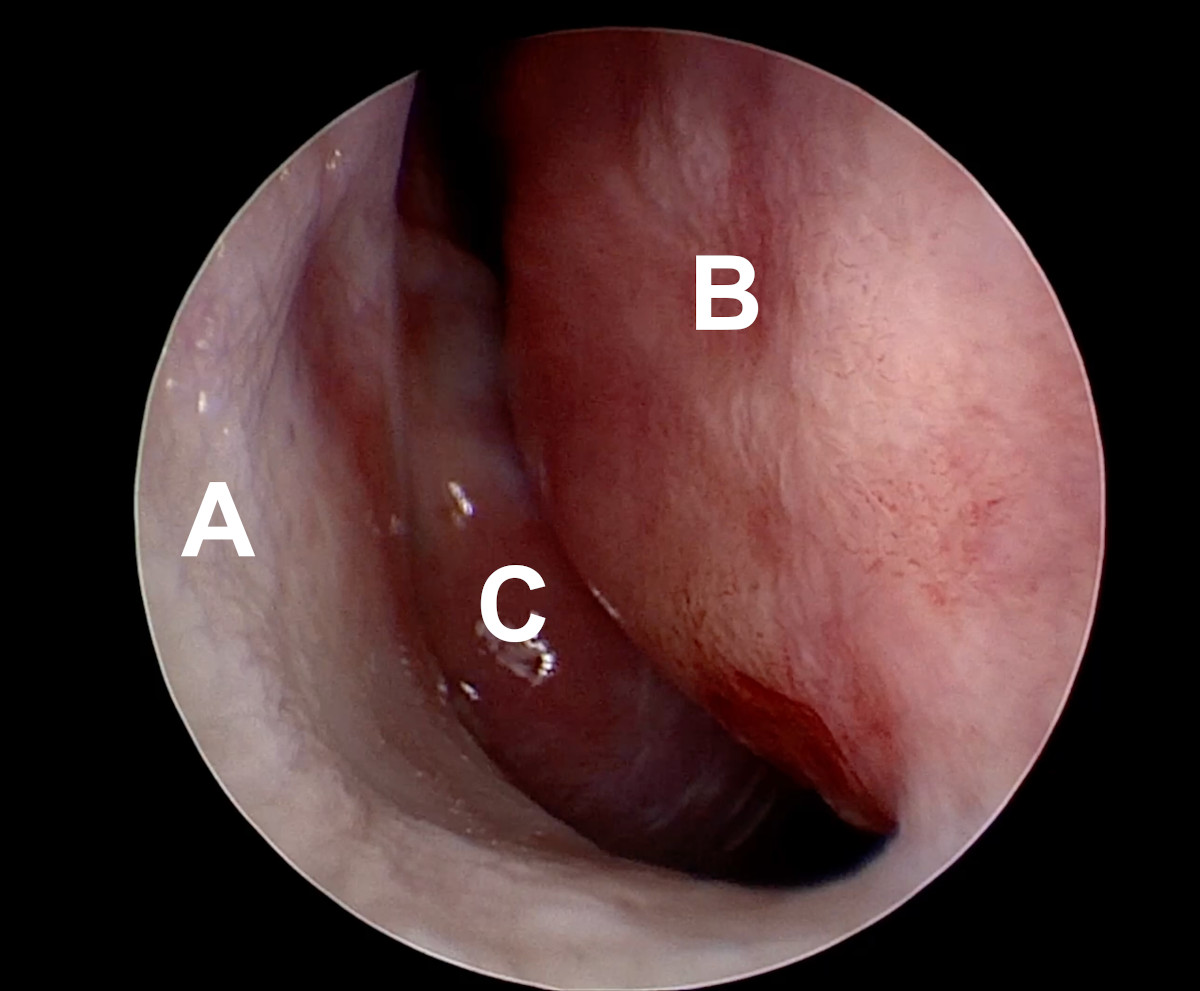
Figure 13. Endoscopic view of the right nasal cavity: septal deviation (A- lateral wall of the nasal cavity, D- deviated nasal septum, C- middle turbinate).
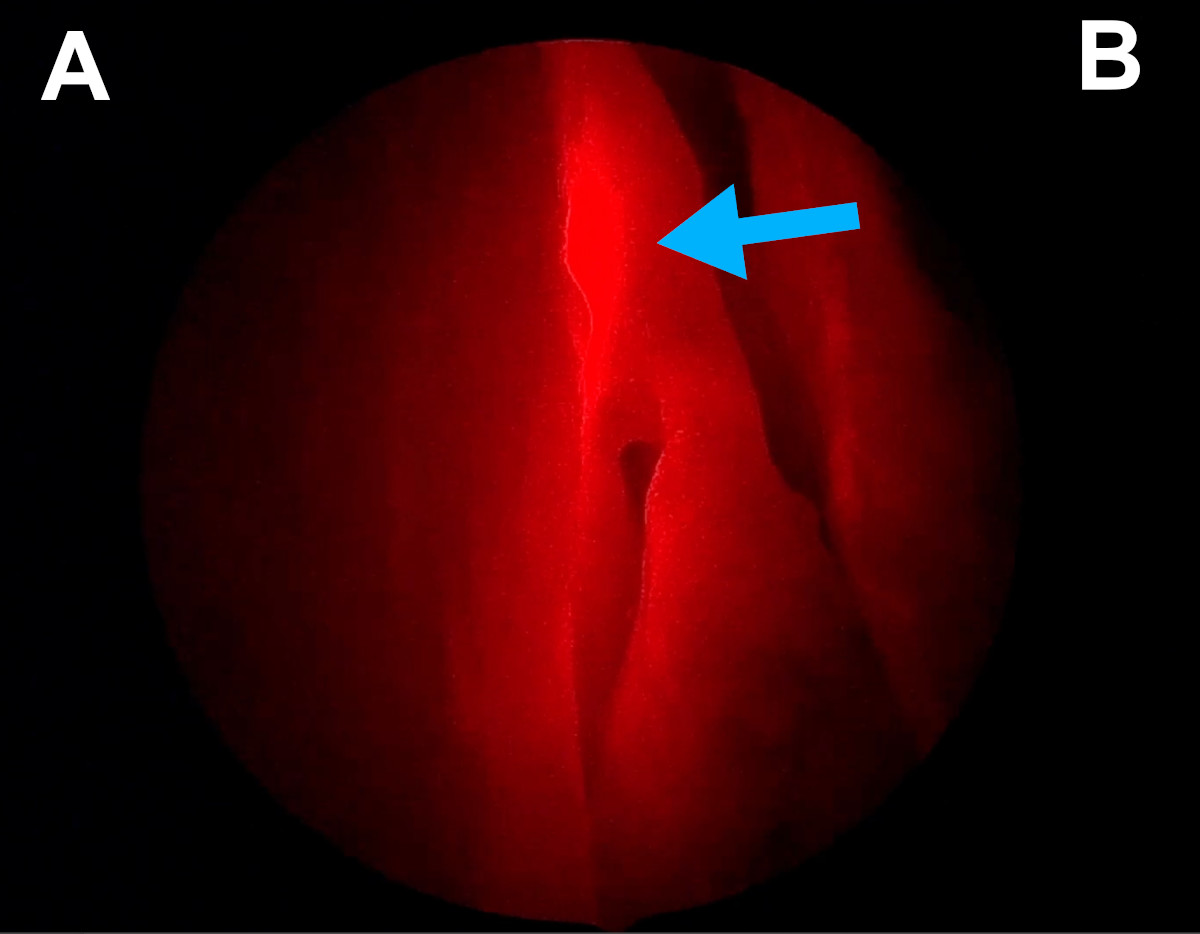
Figure 14. Endoscopic view of the right nasal cavity: light navigation (blue arrow points at the red spot of a light probe introduced into the lacrimal sac through the lacrimal canaliculus; the spot is located at the base of the middle turbinate) [A- lateral wall of the nasal cavity, B- septum].
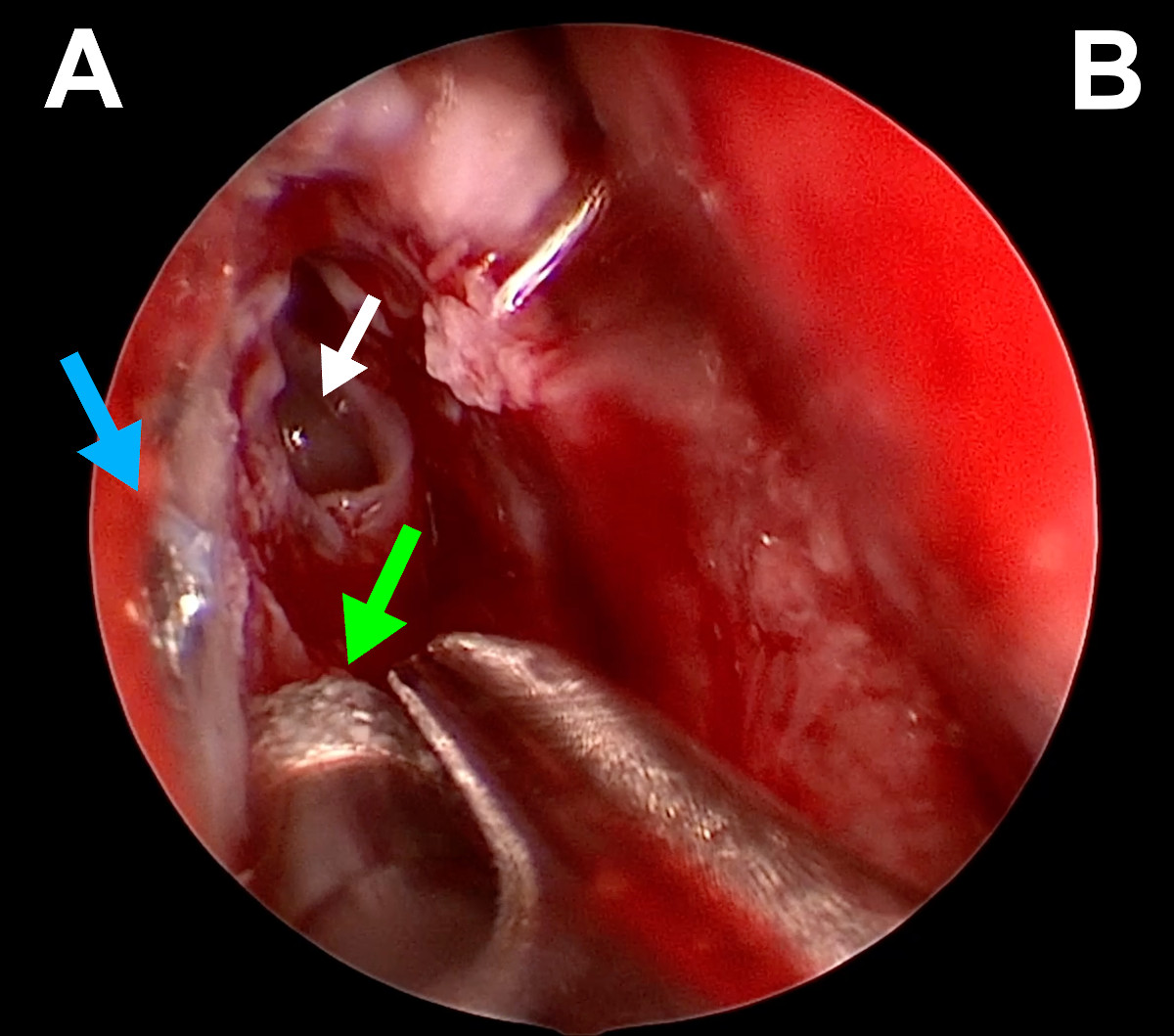
Figure 15. Endoscopic view of the right nasal cavity: green arrow – diamond burr, white arrow – opened agger nasi, blue arrow – tip of a metal bone screw (A- lateral wall of the nasal cavity, B- septum).
CASE 3
The procedure was performed on the left side. The lacrimal sac was found under a thick layer of scar tissue, around 15mm anteriorly to the base of the middle turbinate. Thanks to the previous 3D visualization, it was known that a rim of a metal orbital mesh was located close to the middle turbinate (Fig. 12). It came to the surface during dissection but was then covered with a mucosal flap and tissue glue.
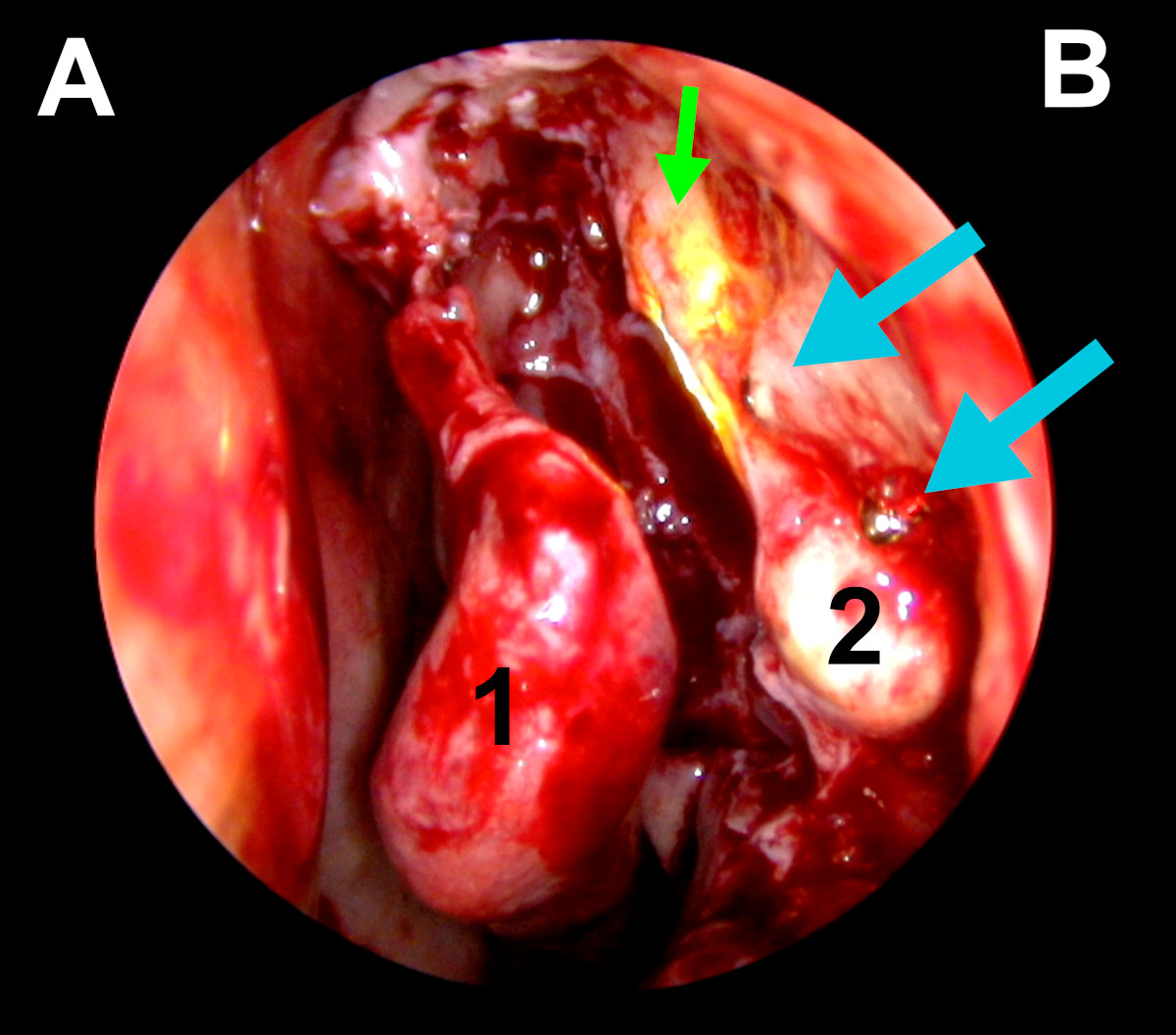
Figure 16. Endoscopic view of the left nasal cavity: blue arrows point on tips of metal bone screws, green arrow- light navigation, 1-middle turbinate, 2- exposed lacrimal sac, (A- septum, B- lateral wall of the nasal cavity).
In all cases proper marsupialization of the lacrimal sac was performed. The lacrimal pathway was intubated with a silicone stent. At the completion of surgery, topical application and circumostial Mitomycin C injection were conducted.
Results
In all of the described cases, lacrimal drainage system remained patent within the follow-up time. Epiphora was absent (Fig. 17-18).
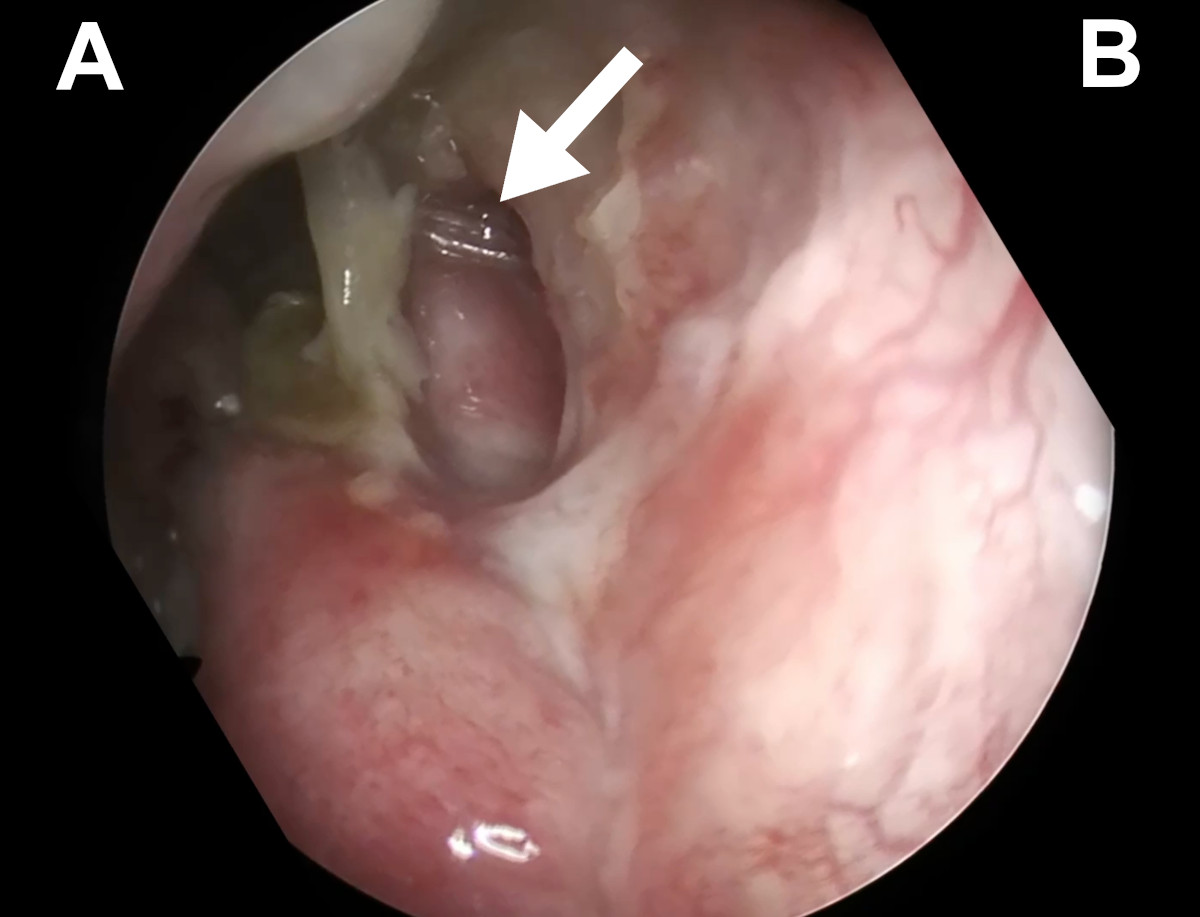
Figure 17. Endoscopic view of the left nasal cavity at 6 weeks postop (Case 1): white arrow points at the silicone stent coming out from a patent ostium (A- nasal septum, B- lateral wall of the nasal cavity).
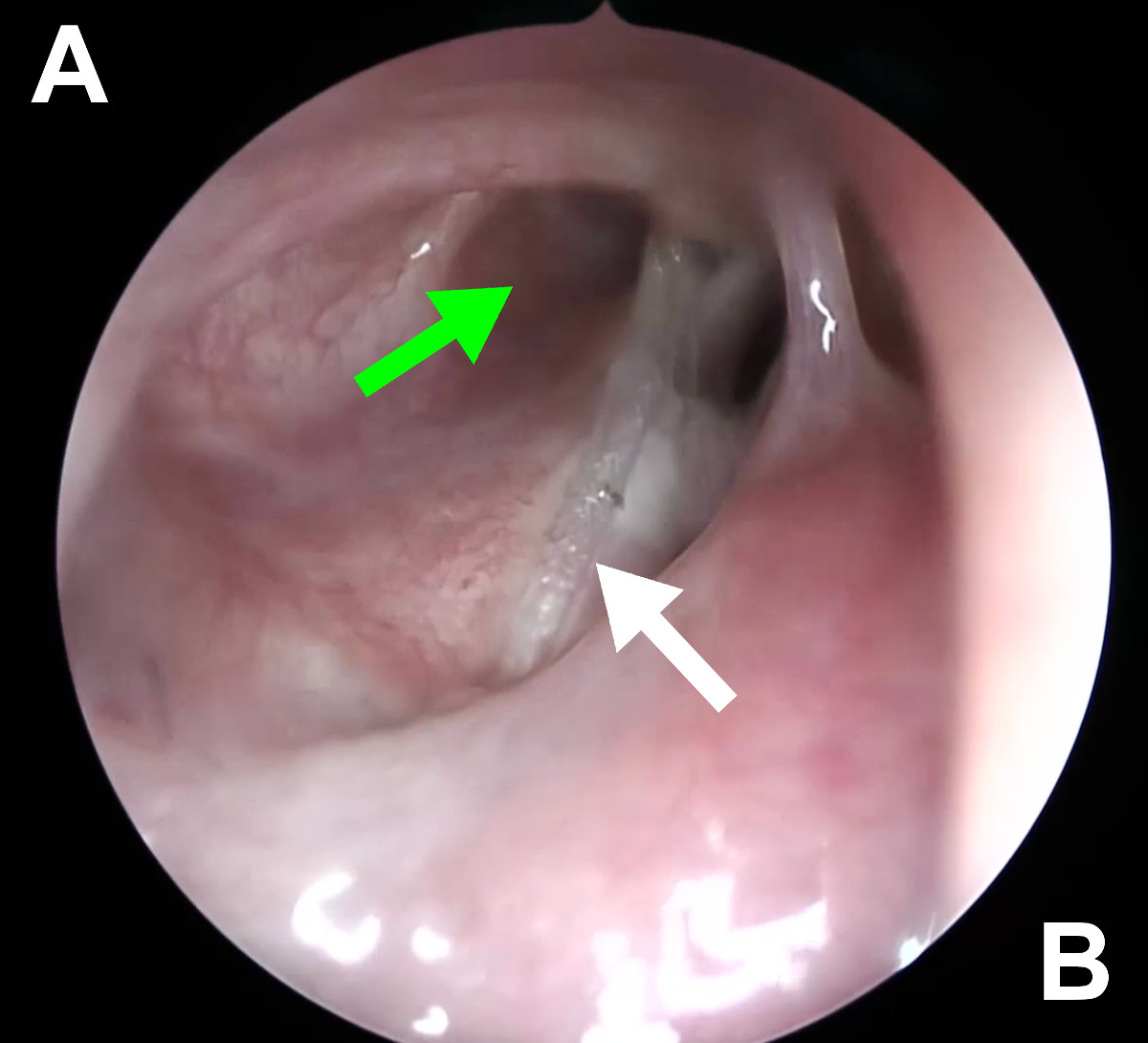
Figure 18. Endoscopic view of the right nasal cavity at 6 weeks postop (Case 2): green arrow - patent ostium, white arrow – silicone stent.
Discussion
Numerous publications indicate that the effectiveness of endoscopic dacryocystorhinostomy (EnDCR) is equal to or even surpasses the effectiveness of external dacryocystorhinostomy (ExDCR)12, 13. This trend results from the development of endoscopy, which allows for better visualization of the surgical field inside the nasal cavity. This is particularly important in atypical, traumatic cases of lacrimal duct obstruction, where the facial anatomy may be significantly altered. Such a situation occurs in the Le Fort fractures. In the past, the endoscopic approach was not recommended for lacrimal duct obstruction resulting from this type of fractures. The method of choice was ExDCR due to what was considered the best surgical access14. However, this approach did not allow for proper evaluation of the surgeon's actions inside the nasal cavity, which is now possible with the use of high-resolution endoscopes. Some authors have even suggested performing dacryocystectomy (DCT) instead of DCR, which is currently considered an inappropriate approach. In the cases described in this publication, the surgeon was able to accurately assess the altered nasal cavity anatomy and make appropriate decisions based on the evolving situation. It allowed for the proper marsupialization of the lacrimal sac under direct endoscopic control.
Ruya indicates that the use of 3D visualization with virtual reality (VR) application can positively impact the surgeon's decision-making during difficult surgeries15. In the three described cases, surgical planning was performed based on conventional imaging and 3D visualization, including VR. Such an approach could have influenced the success of the procedures.
Ali proved that Mitomycin C circumostial injection improves the outcome of EnDCR16. In the discussed cases, 0.02% Mitomycin C was used in two applications: topically and in circumostial injections. This might have had a part in preventing from ostium closure in the postoperative period.
Conclusions
This study shows that endoscopic DCR can be conducted even in the most complex posttraumatic obstructions of the lacrimal pathway. A step-wise approach to such cases with a careful reading of the preoperative CT-DCG and performing a complete marsupialization of the lacrimal sac gives an excellent long-term outcome.
References
1. Ullrich K, Malhotra R, Patel BC. Dacryocystorhinostomy. [Updated
2022 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls
Publishing; 2023 Jan.
2. Perez Y, Patel BC, Mendez MD. Nasolacrimal Duct Obstruction. [Updated
2023 Jan 31]. In: StatPearls [Internet]. Treasure Island (FL):
StatPearls Publishing; 2023 Jan.
3. Nowak R, Rekas M, Gospodarowicz IN, Ali MJ. Long-term outcomes of
primary transcanalicular laser dacryocystorhinostomy. Graefes Arch Clin
Exp Ophthalmol. 2021 Aug;259(8):2425-2430. doi:
10.1007/s00417-021-05165-5. Epub 2021 Mar 26. PMID: 33770269.
4. Mukherjee B, Dhobekar M. Traumatic nasolacrimal duct obstruction:
clinical profile, management, and outcome. Eur J Ophthalmol. 2013
Sep-Oct;23(5):615-22. doi: 10.5301/ejo.5000256. Epub 2013 Mar 20. PMID:
23516252.
5. Mukherjee B, Dhobekar M. Traumatic Nasolacrimal Duct Obstruction:
Clinical Profile, Management, and Outcome. European Journal of
Ophthalmology. 2013;23(5):615-622. doi:10.5301/ejo.5000256.
6. Keren S, Abergel A, Manor A, Rosenblatt A, Koenigstein D, Leibovitch
I, Ben Cnaan R. Endoscopic dacryocystorhinostomy: reasons for failure.
Eye (Lond). 2020 May;34(5):948-953. doi: 10.1038/s41433-019-0612-y. Epub
2019 Oct 8. PMID: 31595028; PMCID: PMC7182564.
7. Goodmaker C, Hohman MH, De Jesus O. Naso-Orbito-Ethmoid Fractures.
[Updated 2023 Mar 1]. In: StatPearls [Internet]. Treasure Island (FL):
StatPearls Publishing; 2023 Jan.
8. Patel BC, Wright T, Waseem M. Le Fort Fractures. [Updated 2022 Sep
12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls
Publishing; 2023 Jan.
9. Wormald PJ. Powered endoscopic dacryocystorhinostomy. Laryngoscope.
2002 Jan;112(1):69-72. doi: 10.1097/00005537-200201000-00013. PMID:
11802041.
10. Ali MJ, Psaltis AJ, Murphy J, Wormald PJ. Powered endoscopic
dacryocystorhinostomy: a decade of experience. Ophthalmic Plast Reconstr
Surg. 2015 May-Jun;31(3):219-21. doi: 10.1097/IOP.0000000000000261.
PMID: 25162414.
11. Nowak R, Ali MJ. Experience of the First Three Years of Independent
Practice Following Surgical Training: Time Taken and Long-Term Outcomes
of Powered Endoscopic Dacryocystorhinostomy. Semin Ophthalmol. 2023 Mar
29:1-5. doi: 10.1080/08820538.2023.2195025. Epub ahead of print. PMID:
36992526.
12. Jung SK, Kim YC, Cho WK, Paik JS, Yang SW. Surgical outcomes of
endoscopic dacryocystorhinostomy: analysis of 1083 consecutive cases.
Can J Ophthalmol. 2015 Dec;50(6):466-70. doi:
10.1016/j.jcjo.2015.08.007. PMID: 26651307.
13. Rizvi SA, Sharma SC, Tripathy S, Sharma S. Management of traumatic
dacryocystitis and failed dacryocystorhinostomy using silicone lacrimal
intubation set. Indian J Otolaryngol Head Neck Surg. 2011
Jul;63(3):264-8. doi: 10.1007/s12070-011-0230-x. Epub 2011 Apr 17. PMID:
22754807; PMCID: PMC3138957.
14. Ruyra X, Permanyer E, Huguet M, Maldonado G. Use of virtual reality
for procedural planning of transcatheter aortic valve replacement.
Interact Cardiovasc Thorac Surg. 2022 Oct 10;35(5):ivac248. doi:
10.1093/icvts/ivac248. PMID: 36205608; PMCID: PMC9639804.
15. Singh, Manpreet M.D.; Ali, Mohammad Javed F.R.C.S.; Naik, Milind N.
M.D.. Long-Term Outcomes of Circumostial Injection of Mitomycin C
(COS-MMC) in Dacryocystorhinostomy. Ophthalmic Plastic and
Reconstructive Surgery 31(5):p 423-424, September/October 2015. | DOI:
10.1097/IOP.0000000000000491.